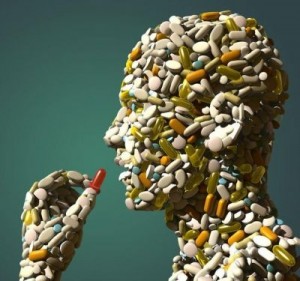
 Note: According Medco Health 1 in 5 American adults are currently taking mind-altering psychiatric drugs such as antidepressants, antipsychotics and anti-anxiety drugs. International drug regulatory agencies have issued warnings that side effects including mania, psychosis, hallucinations, suicidal ideation, diabetes, heart attack, stroke and sudden death as well as severe withdrawal. For more information on documented drug side effects visit CCHR International’s psychiatric drug search engine
Note: According Medco Health 1 in 5 American adults are currently taking mind-altering psychiatric drugs such as antidepressants, antipsychotics and anti-anxiety drugs. International drug regulatory agencies have issued warnings that side effects including mania, psychosis, hallucinations, suicidal ideation, diabetes, heart attack, stroke and sudden death as well as severe withdrawal. For more information on documented drug side effects visit CCHR International’s psychiatric drug search enginePeter Breggin, a leading crusader against the abusive prescription of psychiatric drugs who has been called “the conscience of psychiatry,” presents a pioneering, person-centered approach to psychiatric drug withdrawal in his new book. Psychiatric Drug Withdrawal: A Guide for Prescribers, Therapists, Patients and their Families, published by Springer Publishing Company, is also the first book to establish guidelines and assist the prescriber and therapist in withdrawing their patients from psychiatric drugs.
With increasing evidence that long-term use of psychiatric drugs damages the brain and complicates withdrawal, and with the number of people on psychiatric medication higher than ever, this work comes out at a critical time. The book also anticipates controversial DSM-5 proposals which some say would medicalize normality.
Research shows long-term exposure to psychiatric drugs has proven to be far more dangerous than originally anticipated, and includes the threat of medication-induced obesity, diabetes, heart disease, irreversible abnormal movements, emotional and cognitive disability, and an overall deterioration in the patient’s clinical condition and quality of life. These dangers, among others, have compelled Dr. Breggin to argue that “Nothing in the field of mental health will do more good and reduce more harm than encouraging withdrawal from psychiatric drugs.”
Although therapists are often the first to realize that their patients are overly or unnecessarily medicated, they have been discouraged from voicing their opinions or from participating in medication decision-making, and have been urged or mandated to enforce medication compliance. When a patient is withdrawn from psychiatric medication, it is often done much too rapidly and without regard to the patient’s suffering in the process, since, as Dr. Breggin notes, the dangers of withdrawal are vastly underestimated and overlooked. This resource guides the practitioner in withdrawing patients as safely, expeditiously, and comfortably as possible from psychiatric medication, including patients with long-term exposure to antipsychotic drugs, benzodiazepines, stimulants, antidepressants, and mood stabilizers.
“This model for a patient-centered collaborative team approach not only transforms drug withdrawal, but mental health treatment in general with its greater emphasis on the patient partnership and well-being,” states Dr. Breggin. “It ushers in a new era of patient and family-centered treatment where the goal is no longer a drug-induced holding pattern, but genuine physical and psychological recovery and growth.”

