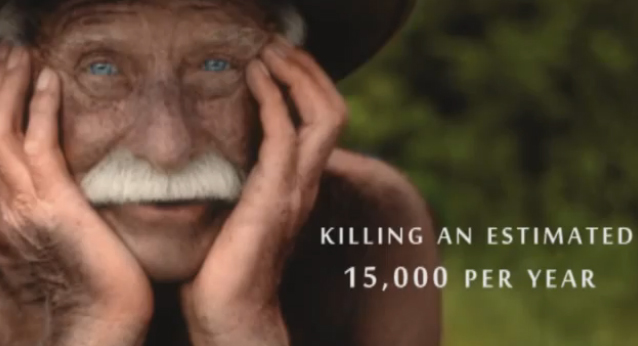
Click to watch video: Each year 350,000 nursing home residents are prescribed powerful antipsychotic drugs, killing an estimated 15,000 per year.
Daily Mail
By Sandra Parsons
February 29, 2012
Let’s imagine for a moment that it’s routine practice in this country to sedate babies who won’t settle: that the more they cry, the more drugs are poured down their tiny throats.
The same treatment, let’s imagine, is also routine for the mentally disabled: whenever they create too much disturbance, we simply cosh them with chemicals.
There would be a national outcry. Heads would roll. Money would be found immediately to train medical staff and carers so that such a scandal could never, ever happen again.
Now let’s stop imagining and face the appalling truth. The nightmare scenario that I’ve just painted is precisely what’s happening to some of the most vulnerable people in the land — the elderly.
A shocking three-year study by Nottingham University has concluded that more than half of all those over 70 who are admitted to hospital have dementia. Yet very few doctors, nurses or healthcare assistants have had any proper training in how to deal with them.
The comments from some of the medical staff questioned for the study make terrifying reading. ‘I just don’t think I’ve ever had any teaching about how to look after people with dementia,’ said one consultant. ‘It’s distressing . . . you feel that you’re not really doing anything other than trying to calm them down,’ added a staff nurse.
People with dementia can’t plan for anything. Understandably, they are often frightened and confused. They feel stigmatised and embarrassed.
The way to help them be calm and happy is to stick to rigid routines that make them feel safe, and by doing activities that they can enjoy in the moment, such as reading aloud. It sounds simple and it is. But it takes time, which is in short supply in acute hospital wards.
If the old and confused aren’t lucky enough to have families who are prepared to make the necessary sacrifices to look after them, they end up lonely, fearful and disturbed. They’re also often malnourished, as they’re frequently unable to feed themselves — and, as we know, most nurses don’t have time (or won’t make time) to help them with their meals.
Is it any wonder that these neglected patients can become aggressive and troublesome? At which point, the medical staff may well resort to anti-psychotic drugs to calm them down.
You’ve only to read the former breakfast TV presenter Fiona Phillips’s account of her father’s terrible last days to realise that no one is immune.
She gave up her highly-paid job so that she could spend more time with him after he was diagnosed with Alzheimer’s. Despite this, and the fact that she was once so well connected politically that Gordon Brown invited her to become one of his health advisers, she was helpless to prevent her father being given the powerful tranquillisers that, as she puts it, robbed him of his life.
Unlike her mother, who tragically also died after suffering the disease, he was often in good spirits. He loved old Fifties hits which, even as his mind went, they’d sing together. Once, when they were dancing to Patsy Cline’s Crazy and it came to the line ‘I’m crazy’, her father laughed as he told her: ‘I am bloody crazy.’ Despite the disease, he was still funny and loveable.
Then, towards the end of last year, his condition deteriorated. The care home Fiona had found kept him only a night before referring him to a psychiatric hospital. There, he was put onto a mixture of drugs so strong that when she next visited, he was like a different person: stooped, shuffling and unresponsive.
When she asked to see a list of his medication, it stretched to two sides of A4 paper. After six days he developed pneumonia and was moved to a general hospital, where, just a few days later, he died.
Like tens of thousands of other elderly people, Fiona Phillips’s father was an honest, decent man who’d worked hard all his life. Unlike the obese — on whom the NHS spends millions a year — he was not ill as a result of his own self-indulgence.
Can it really be so hard to tend to dementia patients with compassion?
Do doctors and nurses need constantly to be reminded that the elderly are human beings?
One consultant in the Nottingham study said that the fact he couldn’t communicate with dementia patients meant he was ‘more veterinary’ in his approach to them.
That remark should chill us all. Tragically, Britain seems to have reached the point where our elderly can expect to be treated no better than animals.

