The Chronicle of Higher Education – September 18, 2011
by By John Horgan
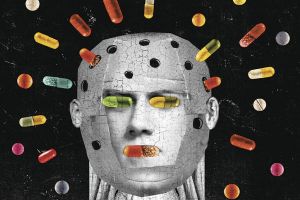
American psychiatry, in collusion with the pharmaceutical industry, is perpetrating what may be the biggest case of iatrogenesis—harmful medical treatment—in history.Dave Plunkert for The Chronicle Review
Three years ago, I was reminded in dramatic fashion of the chasm between psychiatry and more-effective branches of medicine. My 14-year-old son, Mac, while playing lacrosse, emerged from a collision with his right arm askew. I drove him to a local hospital, where an orthopedic surgeon on duty immediately diagnosed the injury: dislocated elbow. He gave Mac an oral and local anesthetic and put him in a portable X-ray machine that showed Mac’s elbow joint on a screen, in real time. Watching the screen, the doctor quickly snapped Mac’s elbow back into place.
Overcome with gratitude to the doctor, I was leading my groggy son out of the hospital when my cellphone rang. An old friend, whom I’ll call Phil, was on the line. He was in the psychiatric ward of a New York hospital, to which his 16-year-old son had been committed. The boy, who was taking antidepressants for depression, had threatened to commit suicide, not for the first time. Thedoctors were recommending electroconvulsive therapy, or ECT.
Knowing that I had written about shock therapy and other psychiatric treatments, Phil asked my opinion. The fact that Phil had called me, a mere journalist, for advice in such a dire situation spoke volumes about the troubles of modern psychiatry.
I first took a close look at treatments for mental illness 15 years ago while researching an article for Scientific American. At the time, sales of a new class of antidepressants, selective serotonin reuptake inhibitors, or SSRI’s, were booming. The first SSRI, Prozac, had quickly become the most widely prescribed drug in the world. Many psychiatrists, notably Peter D. Kramer, author of the best seller Listening to Prozac, touted SSRI’s as a revolutionary advance in the treatment of mental illness. Prozac, Kramer said in a phrase that I hope now haunts him, could make patients “better than well.”
Clinical trials told a different story. SSRI’s are no more effective than two older classes of antidepressants, tricyclics and monoamine oxidase inhibitors. What was even more surprising to me—given the rave reviews Prozac had received from Kramer and others—was that antidepressants as a whole were not more effective than so-called talking cures, whether cognitive behavioral therapy or even old-fashioned Freudian psychoanalysis. According to some investigators, treatments for depression and other common ailments work—if they do work—by harnessing the placebo effect, the tendency of a patient’s expectation of improvement to become self-fulfilling. I titled my article “Why Freud Isn’t Dead.” Far from defending psychoanalysis, my point was that psychiatry has made disturbingly little progress since the heyday of Freudian theory.
In retrospect, my critique of modern psychiatry was probably too mild. According to Anatomy of an Epidemic (Crown Publishers, 2010), by the journalist Robert Whitaker, psychiatry has not only failed to progress but may now be harming many of those it purports to help. Anatomy of an Epidemic has been ignored by most major media. I learned about it only after Marcia Angell, former editor of The New England Journal of Medicine and now a lecturer on public health at Harvard, reviewed the book in The New York Review of Books in June. If Whitaker is right, American psychiatry, in collusion with the pharmaceutical industry, is perpetrating what may be the biggest case of iatrogenesis—harmful medical treatment—in history.
As recently as the 1950s, Whitaker contends, the four major mental disorders—depression, anxiety disorder, bipolar disorder, and schizophrenia—often manifested as episodic and “self limiting”; that is, most people simply got better over time. Severe, chronic mental illness was viewed as relatively rare. But over the past few decades the proportion of Americans diagnosed with mental illness has skyrocketed. Since 1987, the percentage of the population receiving federal disability payments for mental illness has more than doubled; among children under the age of 18, the percentage has grown by a factor of 35.

Between 1985 and 2008, sales of antidepressants and antipsychotics multiplied almost fiftyfold, to $24.2-billion.
This epidemic has coincided, paradoxically, with a surge in prescriptions for psychiatric drugs. Between 1985 and 2008, sales of antidepressants and antipsychotics multiplied almost fiftyfold, to $24.2-billion. Prescriptions for bipolar disorder and anxiety have also swelled. One in eight Americans, including children and even toddlers, is now taking a psychotropic medication. Whitaker acknowledges that antidepressants and other psychiatric medications often provide short-term relief, which explains why so many physicians and patients believe so fervently in the drugs’ benefits. But over time, Whitaker argues, drugs make many patients sicker than they would have been if they had never been medicated.
Whitaker compiles anecdotal and clinical evidence that when patients stop taking SSRI’s, they often experience depression more severe than what drove them to seek treatment. A multination report by the World Health Organization in 1998 associated long-term antidepressant usage with a higher rather than a lower risk of long-term depression. SSRI’s cause a wide range of side effects, including insomnia, sexual dysfunction, apathy, suicidal impulses, and mania—which may then lead patients to be diagnosed with and treated for bipolar disorder.
Indeed, Whitaker suspects that antidepressants—as well as Ritalin and other stimulants prescribed for attention-deficit disorder—have catalyzed the recent spike in bipolar disorder. Though bipolar disorder was relatively rare just a half-century ago, reported rates of it have increased more than a hundredfold, to one in 40 adults. Side effects attributed to lithium and other common medications for bipolar disorder include deficits in memory, learning ability, and fine-motor skills. Similarly, benzodiazepines such as Valium and Xanax, which are prescribed for anxiety, are addictive; withdrawal from these sedatives can cause effects ranging from insomnia to seizures, as well as panic attacks.
Whitaker’s analysis of treatments for schizophrenia is especially disturbing. Antipsychotics, from Thorazine to successors like Zyprexa, cause weight gain, physical tremors (called tardive dyskinesia) and, according to some studies, cognitive decline and brain shrinkage. Before the introduction of Thorazine in the 1950s, Whitaker asserts, almost two-thirds of the patients hospitalized for an initial episode of schizophrenia were released within a year, and most of this group did not require subsequent hospitalization.
Over the past half-century, the rate of schizophrenia-related disability has grown by a factor of four, and schizophrenia has come to be seen as a largely chronic, degenerative disease. A decades-long study by the World Health Organization found that schizophrenic patients fared better in poor nations, such as Nigeria and India, where antipsychotics are sparingly prescribed, than in wealthier regions such as the United States and Europe.
A long-term study by Martin Harrow, a psychologist at the University of Illinois College of Medicine, found an inverse correlation between medication for schizophrenia and positive, long-term outcomes. Beginning in the 1970s, Harrow tracked a group of 64 newly diagnosed schizophrenics. Forty percent of the nonmedicated patients recovered—meaning that they could become self-supporting—versus 5 percent of those who were medicated. Harrow theorized that those who were heavily medicated were sicker to begin with, but Whitaker suggests that the medications may be making some patients sicker.
Several possible objections to Whitaker’s case against psychiatry come to mind. First of all, as Harrow speculates, over time heavily medicated patients may not fare as well as less-medicated patients because the former truly are sicker. Also, the recent surge in mental disability may stem, at least in part, from a decrease in the stigma associated with mental illness, spurring more people to seek and obtain treatment and government assistance. In her review, Marcia Angell called Whitaker’s book “suggestive, if not conclusive,” which seems right to me. At the very least, Whitaker’s claims warrant further investigation.
Between 1985 and 2008, sales of antidepressants and antipsychotics multiplied almost fiftyfold, to $24.2-billion.
Although Whitaker doesn’t address electroconvulsive therapy, its persistence strikes me as yet another symptom of the weakness of modern psychiatry. It fell out of favor in the 1970s, in part because of its negative portrayal in the 1975 film One Flew Over the Cuckoo’s Nest, and yet about 100,000 Americans a year still receive ECT. Studies suggest that the therapy can provide temporary relief from acute depression, but virtually everyone who receives electroconvulsive therapy relapses within a year without further treatment. Proponents claim that ECT has few significant side effects, but this year an FDA panel ruled that ECT should remain classified as a “high-risk” procedure because it can cause persistent memory loss and other side effects. If SSRI’s and other psychiatric medications were truly effective, ECT would long ago have been tossed into the dustbin of failed psychiatric treatments.
So what happened to Phil’s son? When Phil called me, I told him that if my son were suicidally depressed, I’d resist giving him shock treatment unless doctors convinced me there was absolutely no alternative. Phil decided against ECT, and his son, after being released from the hospital, gradually stopped taking antidepressants too. He still struggles with depression, and he smokes more marijuana than Phil would like. But he is healthy enough to be starting college this fall.
http://chronicle.com/article/Are-Psychiatric-Medications/128976/

