Minyanville
By Minyanville Staff
July 28, 2011
When the DSM-II was published in 1980, it became “the bible of psychiatry,” writes Angell, who adds, “but like the real Bible, it depended a lot on something akin to revelation. There are no citations of scientific studies to support its decisions.”
For any mental illness or passing mood swing that may trouble a person, the Diagnostic and Statistical Manual of Mental Disorders — better known as the DSM — has a label and a code. Recurring bad dreams? That may be a Nightmare Disorder, or 307.47. Narcolepsy uses the same digits in a different order: 347.00. Fancy feather ticklers? That sounds like Fetishism, or 302.81. Then there’s the ultimate catch-all for vague sadness or uneasiness, General Anxiety Disorder, or 300.02. That’s a label almost everyone can lay claim to.
These codes are used by doctors, psychologists, and regulators to maintain a mutual language; it’s a handy shorthand system for bureaucratic purposes. But over the past few decades, the staggering, ever-expanding influence of the ever-expanding DSM, which is published by the American Psychiatric Association, has also played a lead role in building wealth and off-label product uses for the major drug manufacturers. In an insightful essay in this week’s New York Review of Books, Marcia Angell, a senior lecturer in social medicine at Harvard Medical School and former Editor in Chief of The New England Journal of Medicine, explains how.
The medical director of the American Psychiatric Association (APA), Melvin Sabshin, declared in 1977 that “a vigorous effort to remedicalize psychiatry should be strongly supported."
Angell’s essay is based on a review of three current books examining the psychiatric industry: The Emperor’s New Drugs: Exploding the Antidepressant Myth, by Irving Kirsch; Anatomy of an Epidemic: Magic Bullets, Psychiatric Drugs, and the Astonishing Rise of Mental Illness in America by Robert Whitaker, and Unhinged: The Trouble with Psychiatry–A Doctor’s Revelations About a Profession in Crisis, by Daniel Carlat. She also cites the DSM-IV, the most recent edition of the manual, while her review traces big pharma’s role in our current mental disorder epidemic to the DSM-III, published in 1980.
To begin, Angell describes the psychiatric profession’s backlash against a developing perception in the 1960s and 1970s that the practice was a “soft” almost pseudo science:
In the late 1970s, the psychiatric profession struck back–hard. As Robert Whitaker tells it in Anatomy of an Epidemic, the medical director of the American Psychiatric Association (APA), Melvin Sabshin, declared in 1977 that “a vigorous effort to remedicalize psychiatry should be strongly supported,” and he launched an all-out media and public relations campaign to do exactly that. Psychiatry had a powerful weapon that its competitors lacked. Since psychiatrists must qualify as MDs, they have the legal authority to write prescriptions. By fully embracing the biological model of mental illness and the use of psychoactive drugs to treat it, psychiatry was able to relegate other mental health care providers to ancillary positions and also to identify itself as a scientific discipline along with the rest of the medical profession. Most important, by emphasizing drug treatment, psychiatry became the darling of the pharmaceutical industry, which soon made its gratitude tangible.
Of the 170 contributors to the current version of the DSM (the DSM-IV-TR), ninety-five had financial ties to drug companies, including all of the contributors to the sections on mood disorders and schizophrenia.
These efforts to enhance the status of psychiatry were undertaken deliberately. The APA was then working on the third edition of the DSM, which provides diagnostic criteria for all mental disorders. The president of the APA had appointed Robert Spitzer, a much-admired professor of psychiatry at Columbia University, to head the task force overseeing the project. The first two editions, published in 1952 and 1968, reflected the Freudian view of mental illness and were little known outside the profession. Spitzer set out to make the DSM-III something quite different. He promised that it would be “a defense of the medical model as applied to psychiatric problems,” and the president of the APA in 1977, Jack Weinberg, said it would “clarify to anyone who may be in doubt that we regard psychiatry as a specialty of medicine.”
When the DSM-II was published in 1980, it became “the bible of psychiatry,” writes Angell, who adds, “but like the real Bible, it depended a lot on something akin to revelation. There are no citations of scientific studies to support its decisions.”
Despite its lack of citations, that DSM named 265 disorders doctors were meant to identify by matching (or mostly matching) a list of symptoms in the book with symptoms described by a patient. The drug companies were quick to see this radical shift in psychiatry as an opportunity. From the 1980s until now, as Angell demonstrates, the drug makers have supported the move away from talk therapy to the drug therapy, which also benefits practitioners, since doling out drugs and tweaking prescriptions earns a psychiatrist more money for less time spent with a patient.
Here Angell explains how companies influence the DSM itself. The bold typeface is ours.
Drug companies are particularly eager to win over faculty psychiatrists at prestigious academic medical centers. Called “key opinion leaders” (KOLs) by the industry, these are the people who through their writing and teaching influence how mental illness will be diagnosed and treated. They also publish much of the clinical research on drugs and, most importantly, largely determine the content of the DSM. In a sense, they are the best sales force the industry could have, and are worth every cent spent on them. Of the 170 contributors to the current version of the DSM (the DSM-IV-TR), almost all of whom would be described as KOLs, ninety-five had financial ties to drug companies, including all of the contributors to the sections on mood disorders and schizophrenia.
The drug industry, of course, supports other specialists and professional societies, too, but Carlat asks, “Why do psychiatrists consistently lead the pack of specialties when it comes to taking money from drug companies?” His answer: “Our diagnoses are subjective and expandable, and we have few rational reasons for choosing one treatment over another.” Unlike the conditions treated in most other branches of medicine, there are no objective signs or tests for mental illness—no lab data or MRI findings—and the boundaries between normal and abnormal are often unclear. That makes it possible to expand diagnostic boundaries or even create new diagnoses, in ways that would be impossible, say, in a field like cardiology. And drug companies have every interest in inducing psychiatrists to do just that.
In addition to the money spent on the psychiatric profession directly, drug companies heavily support many related patient advocacy groups and educational organizations. Whitaker writes that in the first quarter of 2009 alone, “Eli Lilly gave $551,000 to NAMI [National Alliance on Mental Illness] and its local chapters, $465,000 to the National Mental Health Association, $130,000 to CHADD (an ADHD [attention deficit/hyperactivity disorder] patient-advocacy group), and $69,250 to the American Foundation for Suicide Prevention.”
And that’s just one company in three months; one can imagine what the yearly total would be from all companies that make psychoactive drugs. These groups ostensibly exist to raise public awareness of psychiatric disorders, but they also have the effect of promoting the use of psychoactive drugs and influencing insurers to cover them. Whitaker summarizes the growth of industry influence after the publication of the DSM-III as follows:
“In short, a powerful quartet of voices came together during the 1980’s eager to inform the public that mental disorders were brain diseases. Pharmaceutical companies provided the financial muscle. The APA and psychiatrists at top medical schools conferred intellectual legitimacy upon the enterprise. The NIMH [National Institute of Mental Health] put the government’s stamp of approval on the story. NAMI provided a moral authority.”
And now here we are in 2011, with almost everyone we know taking two or three different mood disorder drugs. (This trend is not limited to mental disorder, mind you. See Disease Branding.)
Work started on the DSM-V in 1999, which is due out in 2013. It will contain many new disorders, such as “binge eating” and “restless leg disorder.” It will also expand existing categories by tacking on words like “spectrum” to the end of a known disorder, Angell reports. “It looks as though it will be harder and harder to be normal,” she writes.
But the curtain gets pulled back further still.
In her review of Daniel Carlat’s book, Angell calls attention to the “disillusioned insider’s” frank admission that when he prescribes a drug, his decision process is largely guesswork. Carlat’s view is that although any psychiatrist will acknowledge that he or she has had great success with mental disorder drugs for say, depression or anxiety, no doctor can say with certainty whether the drugs are working or if a placebo effect has taken effect.
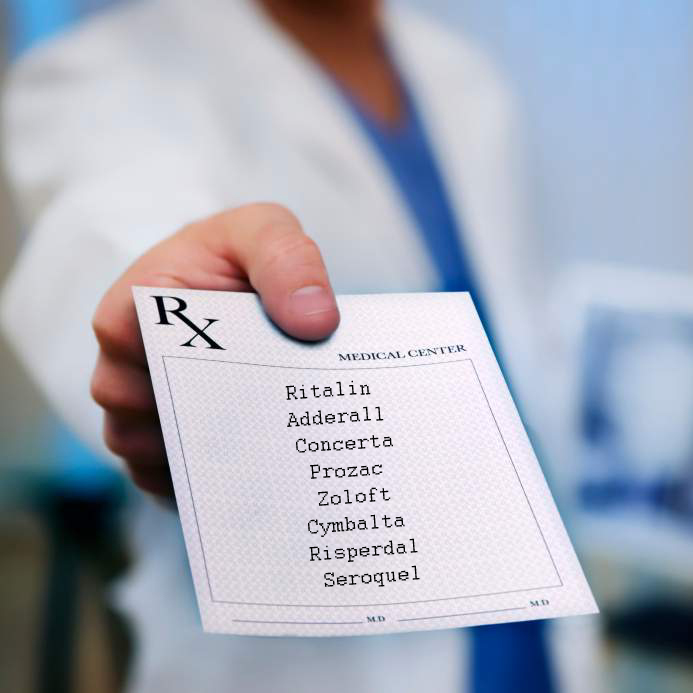
[Carlat’s] work consists of asking patients a series of questions about their symptoms to see whether they match up with any of the disorders in the DSM. This matching exercise, he writes, provides “the illusion that we understand our patients when all we are doing is assigning them labels.” Often patients meet criteria for more than one diagnosis, because there is overlap in symptoms. For example, difficulty concentrating is a criterion for more than one disorder. One of Carlat’s patients ended up with seven separate diagnoses. “We target discrete symptoms with treatments, and other drugs are piled on top to treat side effects.” A typical patient, he says, might be taking Celexa for depression, Ativan for anxiety, Ambien for insomnia, Provigil for fatigue (a side effect of Celexa), and Viagra for impotence (another side effect of Celexa).
As for the medications themselves, Carlat writes that “there are only a handful of umbrella categories of psychotropic drugs,” within which the drugs are not very different from one another. He doesn’t believe there is much basis for choosing among them. “To a remarkable degree, our choice of medications is subjective, even random. Perhaps your psychiatrist is in a Lexapro mood this morning, because he was just visited by an attractive Lexapro drug rep.”
Messy. And, of course, the whole system is now being exported to China and other countries where the middle class is growing and the mental health industry is still in a developing stage.
Angell’s latest book is The Truth About the Drug Companies: How They Deceive Us and What to Do About It.
Read the rest of her essay, which examines the controversial use of brain chemistry drugs to treat children, here.
http://www.minyanville.com/dailyfeed/2011/07/25/harvard-expert-links-our-mental/