Wired—December 27, 2010
by Gary Greenberg
Every so often Al Frances says something that seems to surprise even him. Just now, for instance, in the predawn darkness of his comfortable, rambling home in Carmel, California, he has broken off his exercise routine to declare that “there is no definition of a mental disorder. It’s bullshit. I mean, you just can’t define it.” Then an odd, reflective look crosses his face, as if he’s taking in the strangeness of this scene: Allen Frances, lead editor of the fourth edition of the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (universally known as the DSM-IV), the guy who wrote the book on mental illness, confessing that “these concepts are virtually impossible to define precisely with bright lines at the boundaries.” For the first time in two days, the conversation comes to an awkward halt.
But he recovers quickly, and back in the living room he finishes explaining why he came out of a seemingly contented retirement to launch a bitter and protracted battle with the people, some of them friends, who are creating the next edition of the DSM. And to criticize them not just once, and not in professional mumbo jumbo that would keep the fight inside the professional family, but repeatedly and in plain English, in newspapers and magazines and blogs. And to accuse his colleagues not just of bad science but of bad faith, hubris, and blindness, of making diseases out of everyday suffering and, as a result, padding the bottom lines of drug companies. These aren’t new accusations to level at psychiatry, but Frances used to be their target, not their source. He’s hurling grenades into the bunker where he spent his entire career.
One influential advocate for diagnosing bipolar disorder in kids failed to disclose money he received from the makers of the bipolar drug Risperdal.
As a practicing psychotherapist myself, I can attest that this is a startling turn. But when Frances tries to explain it, he resists the kinds of reasons that mental health professionals usually give each other, the ones about character traits or personality quirks formed in childhood. He says he doesn’t want to give ammunition to his enemies, who have already shown their willingness to “shoot the messenger.” It’s not an unfounded concern. In its first official response to Frances, the APA diagnosed him with “pride of authorship” and pointed out that his royalty payments would end once the new edition was published—a fact that “should be considered when evaluating his critique and its timing.”
Frances, who claims he doesn’t care about the royalties (which amount, he says, to just 10 grand a year), also claims not to mind if the APA cites his faults. He just wishes they’d go after the right ones—the serious errors in the DSM-IV. “We made mistakes that had terrible consequences,” he says. Diagnoses of autism, attention-deficit hyperactivity disorder, and bipolar disorder skyrocketed, and Frances thinks his manual inadvertently facilitated these epidemics—and, in the bargain, fostered an increasing tendency to chalk up life’s difficulties to mental illness and then treat them with psychiatric drugs.
The insurgency against the DSM-5 (the APA has decided to shed the Roman numerals) has now spread far beyond just Allen Frances. Psychiatrists at the top of their specialties, clinicians at prominent hospitals, and even some contributors to the new edition have expressed deep reservations about it. Dissidents complain that the revision process is in disarray and that the preliminary results, made public for the first time in February 2010, are filled with potential clinical and public relations nightmares. Although most of the dissenters are squeamish about making their concerns public—especially because of a surprisingly restrictive nondisclosure agreement that all insiders were required to sign—they are becoming increasingly restive, and some are beginning to agree with Frances that public pressure may be the only way to derail a train that he fears will “take psychiatry off a cliff.”
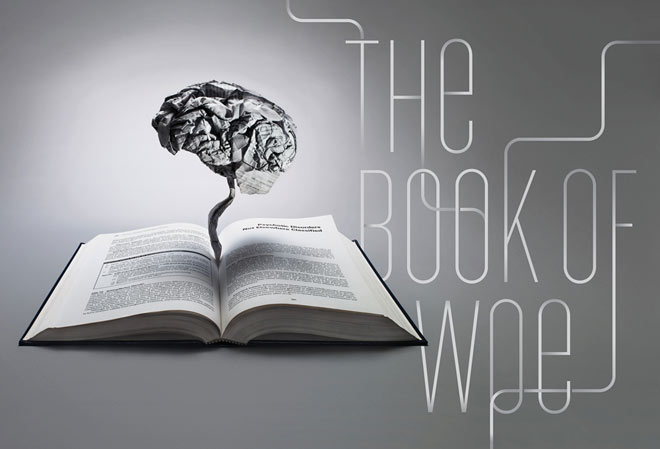
At stake in the fight between Frances and the APA is more than professional turf, more than careers and reputations, more than the $6.5 million in sales that the DSM averages each year. The book is the basis of psychiatrists’ authority to pronounce upon our mental health, to command health care dollars from insurance companies for treatment and from government agencies for research. It is as important to psychiatrists as the Constitution is to the US government or the Bible is to Christians. Outside the profession, too, the DSM rules, serving as the authoritative text for psychologists, social workers, and other mental health workers; it is invoked by lawyers in arguing over the culpability of criminal defendants and by parents seeking school services for their children. If, as Frances warns, the new volume is an “absolute disaster,” it could cause a seismic shift in the way mental health care is practiced in this country. It could cause the APA to lose its franchise on our psychic suffering, the naming rights to our pain.
This is hardly the first time that defining mental illness has led to rancor within the profession. It happened in 1993, when feminists denounced Frances for considering the inclusion of “late luteal phase dysphoric disorder” (formerly known as premenstrual syndrome) as a possible diagnosis for DSM-IV. It happened in 1980, when psychoanalysts objected to the removal of the word neurosis—their bread and butter—from the DSM-III. It happened in 1973, when gay psychiatrists, after years of loud protest, finally forced a reluctant APA to acknowledge that homosexuality was not and never had been an illness. Indeed, it’s been happening since at least 1922, when two prominent psychiatrists warned that a planned change to the nomenclature would be tantamount to declaring that “the whole world is, or has been, insane.”
Some of this disputatiousness is the hazard of any professional specialty. But when psychiatrists say, as they have during each of these fights, that the success or failure of their efforts could sink the whole profession, they aren’t just scoring rhetorical points. The authority of any doctor depends on their ability to name a patient’s suffering. For patients to accept a diagnosis, they must believe that doctors know—in the same way that physicists know about gravity or biologists about mitosis—that their disease exists and that they have it. But this kind of certainty has eluded psychiatry, and every fight over nomenclature threatens to undermine the legitimacy of the profession by revealing its dirty secret: that for all their confident pronouncements, psychiatrists can’t rigorously differentiate illness from everyday suffering. This is why, as one psychiatrist wrote after the APA voted homosexuality out of the DSM, “there is a terrible sense of shame among psychiatrists, always wanting to show that our diagnoses are as good as the scientific ones used in real medicine.”
Since 1980, when the DSM-III was published, psychiatrists have tried to solve this problem by using what is called descriptive diagnosis: a checklist approach, whereby illnesses are defined wholly by the symptoms patients present. The main virtue of descriptive psychiatry is that it doesn’t rely on unprovable notions about the nature and causes of mental illness, as the Freudian theories behind all those “neuroses” had done. Two doctors who observe a patient carefully and consult the DSM’s criteria lists usually won’t disagree on the diagnosis—something that was embarrassingly common before 1980. But descriptive psychiatry also has a major problem: Its diagnoses are nothing more than groupings of symptoms. If, during a two-week period, you have five of the nine symptoms of depression listed in the DSM, then you have “major depression,” no matter your circumstances or your own perception of your troubles. “No one should be proud that we have a descriptive system,” Frances tells me. “The fact that we do only reveals our limitations.” Instead of curing the profession’s own malady, descriptive psychiatry has just covered it up.
Read the rest of the article here: